48 YEAR OLD FEMALE PRESENTING WITH PAIN IN ABDOMEN AND DISTENSION.
E LOG GENERAL MEDICINE
Hi, I am Rishitha, 3rd Sem Medical Student. This is an online e-log book to discuss our patient's health data shared after taking his/her/guardian's consent . This also reflects patient centered care and online learning portfolio.
This E-log book also reflects my patient-centered online learning portfolio and of course, your valuable inputs and feedbacks are most welcome through the comments box provided at the very end. HAPPY READING!
* This is an ongoing case. I am in the process of updating and editing this ELOG as and when required.
*Elog made under guidance of Dr. Bhavya (Intern)
CASE SHEET
48 YEAR OLD FEMALE PRESENTING WITH PAIN IN ABDOMEN AND DISTENSION.
This is a case of 48 year old female who is a regular alochol consumer, came with the chief complaints of upper abdominal pain and distension since 20 days.
CHIEF COMPLAINTS
- c/o upper abdominal pain and distension from past 20 days
- SOB grade III - IV from past 15 days. Patient was asymptotic 4 months back and then she had developed SOB grade III - IV for which she went to a local hospital.
- Patient was asymptotic 20 days back and has been doing her routine work without any limitations.
- She then had developed abdominal pain and distension.
- And SOB grade III - IV associated with orthopnoea, 15 days back, where she visited a local hospital.
- And was prescribed medication and used the treatment for 10 days and stopped.
- Heart palpitations sound positive.
- No h/o chest pain / giddiness/ syncope/ cough
- No h/o vomiting
- No h/o diarrhoea
- No other specific complaints.
- k/c/o
- Diabetes Mellitus
- Appetite is Lost
- Having Mixed diet
- Bowels - Regular
- Micturition - Normal
- No known allergies
- Regular consumer of Alcohol.
- No other habits or addictions.
- No relevant treatment history.
Pallor: - Not seen.
Vitals
Temperature - 98.6 °F
Pulse rate - 142/ min
RR - 18/ min
BP - 110/70 mm/Hg
SpO2 - 98%
GRBS - 212 mg%
Systemic Examination
1. CVS
- No thrills
- S1 and S2 heard
- No murmers
- No dyspnoea
- No wheezing
- Position of trachea - central
- Vesicular breath sounds heard
- No adventitious sounds
- Shape - Scaphoid
- No palpable mass
- Normal hernial orifices
- No free fluid
- No Bruits
- Liver is not palpable
- Spleen is not palpable
- Bowel sounds heard.
- Patient is Conscious and Coherent
- Normal Speech
- No signs of meningeal irritation
- Cranial Nerves intact
- Motor system reflexes are normal
- Glasgow scale - 15/15
- Normal Gait
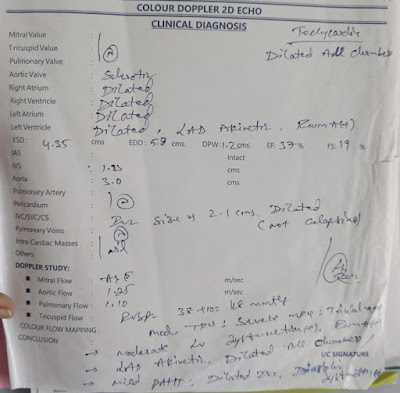
PROVISIONAL DIAGNOSIS
Persistent Atrial Fibrillation (AF) with RVR, associated with FVR (Forearm Vascular Resistance),
HfrEf 2° to CAD.
INVESTIGATIONS TO BE ORDERED
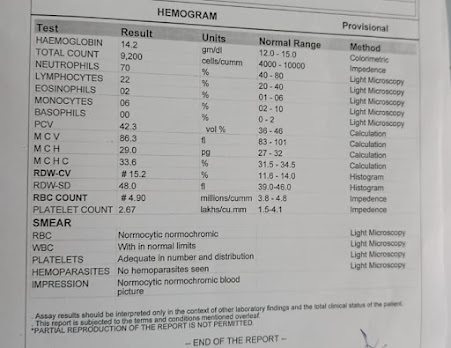
1. Hemogram
2. CUE
- Fluid restriction < 1 L/day
- Salt restriction < 2 gm/day
- Inj LASI 40 mg
- Tab MET 25 mg
- Inj HAI /s/c/ TID
- Tab. DIGOXIN 0.25 mg/OD
- Inj CLEXANE 40 mg.
- Inj LASIX 40 mg
- Tab. Met Xl 25 mg
- Tab. Ecosporin
- Tab. Digoxin 0.25 mg
- Tab. Clexane 40 mg
- Tab. HAI
- Fluid restriction < 1 L/day
- Salt restriction < 2 gm/day
- Inj LASIX 40 mg
- Tab. Met XL 25 mg
- Tab. Ecosporin
- Tab. Digoxin 0.25 mg
- Tab. Clexane 40 mg
- Tab. LASIX
- Tab. Met XL
- Inj. CLEXANE 40 mg
- Tab. Ecosporin
- Tab. Digoxin 0.25 mg
- Syprup Lactulose 15 ml
- Tab. METFORMIN 500 mg
- Fluid restriction < 1 L/day
- Salt restriction < 2 gm/day
- Inj LASIX 40 mg
- Tab. Met XL 25 mg
- Tab. Ecosporin
- Tab. METFORMIN 500 mg.
- Syprup Lactulose 15 ml





















Comments
Post a Comment